Bolivia, October 2012. Traveling alone in a run-down mining town, a several hours bus ride from the nearest major city, Zack Crockett was in trouble.
An American abroad, and future Priceonomics writer, Zack was taking a short stay in the town of Potosí — a historic boom town that was once the richest city in South America, and is now in Zack’s words “a dying city.” On his way back to his hostel, he had spotted a large, mangy dog on a stoop. “I just remember making eye contact with it,” Zack says. “It had these bulbous, disgusting red eyes.”
Zack looked away, and the dog darted forward without warning, and sunk its teeth into his calf. “It didn’t even bark.”
Within seconds, Zack was being chased by all the dogs in the neighborhood. He had to hop a fence to shake them off, and then he got down to the tricky business of survival.
Zack was pretty convinced the dog that bit him had rabies. And if Zack caught rabies from the dog, and went untreated, he was in for a pretty gnarly end: First, he’d appear to get the flu. Then, he’d start exhibiting some of rabies’ neurological symptoms, which include insomnia, paranoia, anxiety, terror, hallucinations, and partial paralysis. From the New York Times:
“[At rabies’ peak], the patient’s whole nervous system seems to be aroused. He is in a state of extreme agitation and has frightening hallucinations. His face is a mask of terror. He shouts incomprehensibly at the top of his distorted voice. His body is racked with tremors or spasms. He may struggle frantically and powerfully to free himself from constraints and try to escape from the room.”
Finally, he’d slip into delirium and full paralysis before dying.
Rabies is a horrible disease that nobody should ever have to suffer from. In fact, they literally shouldn’t — the technology exists to completely wipe human rabies off the map. People in most developed countries rarely get rabies, which is not to say that people rarely get rabies anymore: the World Health Organization (WHO) estimates it claims 60,000 lives a year.
Unfortunately most of the people who do get rabies, or are at risk of getting rabies, are very poor. The economic incentives to eliminate the disease globally, or to improve treatment, or to create better infrastructure to administer treatment, just don’t exist. That makes rabies a Neglected Tropical Disease.
“Neglected diseases fall outside the market,” Mary Moran, World Health Organization (WHO) expert on research and development wrote in the Financial Times last fall. “They aren’t commercial and consequently patents and profit play no role in stimulating innovation. Like all non-commercial areas, these diseases are the responsibility of governments and philanthropy (including industry philanthropy).”
But if governments and philanthropists were doing this effectively, these diseases would not be “neglected.” WHO has an official Neglected Tropical Diseases list, from which the “big two” tropical diseases, HIV and malaria, are conspicuously absent. That’s because HIV and malaria are kind of enjoying the global spotlight: there are large foundations, research, and treatment efforts dedicated to them and their sufferers. It’s a strange thing to say about deadly illnesses but HIV and malaria are, in some sense, kind of glamorous.
There’s debate on what officially qualifies as a Neglected Tropical Disease, but this is the WHO’s list:
Chagas disease
Human African trypanosomiasis (sleeping sickness)
Leishmaniases
Buruli ulcer
Leprosy (Hansen disease)
Trachoma
Yaws
Cysticercosis/Taeniasis
Dracunculiasis (guinea-worm disease)
Echinococcosis
Foodborne trematodiases
Lymphatic filariasis
Onchocerciasis (river blindness)
Schistosomiasis
Soil-transmitted helminthiases
Dengue and Chikungunya
Rabies
These diseases have never been in a GAP commercial. In fact, you’ve probably never even heard of many of them, or at least not thought of them as something that “people still get.” But they do.
“Neglected tropical diseases blight the lives of a billion people worldwide,” the WHO writes, “and threaten the lives of millions more.”
This translates to a big ethical and economic dilemma for the world today. For Zack Crockett in October of 2012, it meant he was in big, big trouble. Another classic feature of a Neglected Tropical Disease is that, in the areas it poses the biggest threat, medical infrastructure is woefully insufficient to combat it. A police officer told Zack that Potosí didn’t have the medical facilities to administer the treatment, which is extremely time-sensitive, locally. He would have to go to a hospital in La Paz, several hours bus ride away.
A History of Neglect
Rabies is one of the oldest diseases known to man. Even the ancient Mesopotamians knew it was spread by dogbite: the Codex of Eshnunna — dating from 1930 BC — states that a person whose dog shows signs of rabies should take measures to prevent the dog from biting, and fines the dog owner if someone bitten by the rabid dog dies. The word “rabies” means “rage” in Latin.
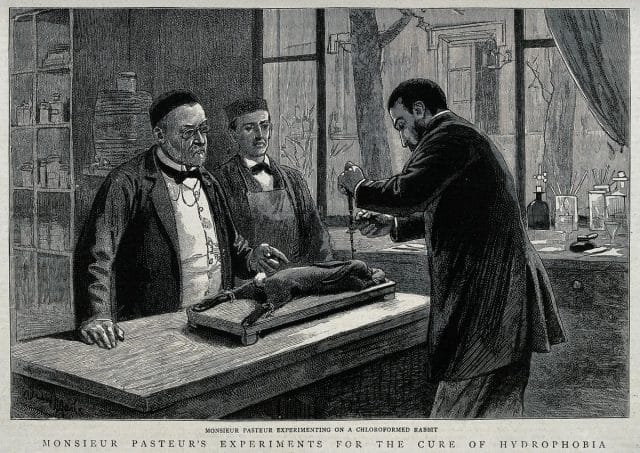
Given such early knowledge of the disease and its transmission, it makes sense that one of the first vaccines ever developed and tested was a rabies vaccine. The famed father of microbiology and pasteurization, Louis Pasteur, and his colleagues developed the first successful rabies vaccine from the desiccated nerve tissue of several highly rabid rabbits. Desiccation weakened the virus over time — and it was with this weakened strain that they were able to immunize 50 dogs.
In 1885, when the vaccine had only been tested on dogs, someone brought Pasteur the 9-year-old Joseph Meister, who had been badly mauled by a rabid dog two days before. From the Journal of Neurology, Neurosurgery & Psychiatry:
“The child was given 13 further inoculations in 10 days with [emulsions from portions of a rabid rabbit’s spinal cord] that were progressively fresher (more virulent), until after three months and three days [Pasteur] announced that the child’s life was now out of danger and his health appeared excellent.”
Pasteur had at first been hesitant to administer the treatment, particularly because he was not a licensed physician and could have faced prosecution. When the treatment worked, however, he was hailed as a hero, and sought out by the victims of rabid animals worldwide. A group of 19 Russian peasants from Smolnik, who had been attacked by a rabid wolf, took a two week train trip despite their injuries to seek Pasteur’s help. His vaccine saved all but 3 of them. By 1886 he had treated 350 patients from Western Europe, America, and Russia.
While human immunization with an artificial vaccine was a major medical breakthrough, it turned out that the real solution to rabies as a public health problem was to vaccinate dogs. The UK successfully eliminated rabies from all animal populations, except bats, by 1922. The trick to eliminating human rabies is to vaccinate upwards of 70% of the dog population — upwards of 90% of human rabies cases come from dogs. Hardly anyone gets rabies in developed countries, now, because mandatory vaccinations in domestic animals, and culling programs for feral ones, have all but eliminated it from canine populations.
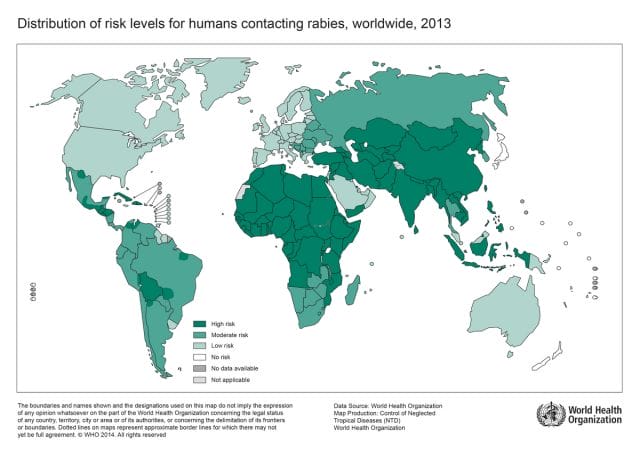
Bolivia is a “high risk” region; Rabies prevalence, WHO
It was a huge triumph for humans and dogs everywhere! And then, rabies continued to exist. “Despite evidence that control of canine rabies […] can reduce the incidence of human rabies to very low numbers,” the European Federation of Pharmaceutical Industries and Associations (EFPIA) writes, “for the time being, the cost of these programmes prohibits their full implementation in much of the developing world.”
This is typical of a Neglected Tropical Disease — it is understood how to fight it, or at least what the next steps are, but the economic structure just isn’t there to carry them out.
“Human deaths from rabies,” EFPIA also notes, “occur in countries with inadequate public health resources, limited access to preventive treatment, few diagnostic facilities and almost no rabies control programmes.” As luck would have it, Zack was smack dab in the middle of a “high risk” rabies region.
Modern Day Rabies Treatment
The city of Potosí
This is what rabies treatment looked like in Bolivia, 2012: Zack took an overnight bus to La Paz, arriving on a Sunday, only to find that all the hospitals in La Paz that could administer the treatment were closed on Sundays. He would have to wait another 24 hours.
The clock was ticking. Post-exposure rabies treatment (i.e. the treatment for a rabid bite) works by immunizing the patient’s body before the virus spreads too far. It’s a race between the vaccination and the actual virus. The patient’s immune system has to build enough antibodies to the vaccination’s weakened strain of rabies to overpower the bite’s infection before it takes hold of the Central Nervous System. As you can imagine, the sooner this treatment is administered, the better.
There is currently no diagnostic for whether someone, before they show symptoms, will get rabies. The doctor who treated Zack in La Paz told him he had two options: the first was to get the hospital’s standard post-exposure treatment — a series of five shots of the weakened virus over a period of 25 days.
The second option was to go back to Potosí and find the dog. If the dog was dead, it probably had rabies: Zack should come back to La Paz and receive treatment. If the dog was still alive, it might still have had rabies: Zack should kill it, and bring a piece of its flesh back to La Paz for analysis. Then, if the flesh tested positive, Zack should receive treatment. This pilgrimage would of course eat up more valuable time, put his life at greater risk, and might require killing a deranged dog. But could save him the pain and price of unnecessary treatment.
Zack also had a third option: to roll the dice and ignore it. The WHO thinks this is actually a much more common choice among rabies victims than we might expect.
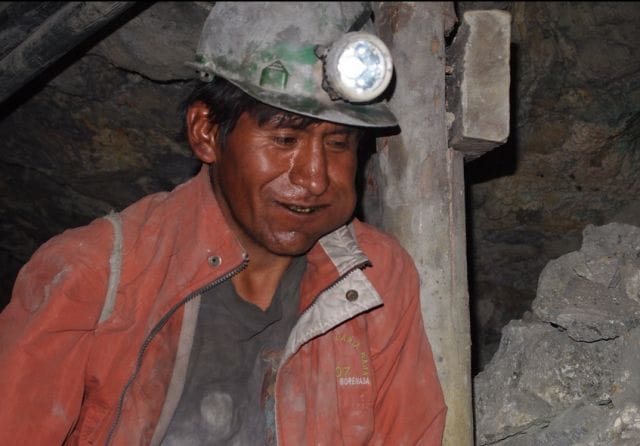
A miner in Potosí
One reason for this is rabies treatment is expensive. In Bolivia, all told, it would cost about $600 US. As we’ve pointed out, regions of high rabies prevalence tend to be very poor. Families often have to borrow money to be able to afford treatment, those who can’t, go untreated for lack of funds.
Rabies is also weirdly easy to ignore, at least for a while. It has near 100% fatality rate, once symptoms have developed, which usually takes a few weeks. But, depending on the location of the bite, the virulence of the strain, and the victim’s immune system, the disease can lie latent for years before symptoms emerge. It’s completely possible to be bitten by a rabid animal, appear to make a full recovery, and then be suddenly struck by a mysterious illness years later, suffer intensely for weeks, and die.
This is tragic for the victims and their families, and also problematic from a global health perspective: it leads to underreporting, which, the WHO says “prevents mobilization of resources from the international community for the elimination of human dog-mediated rabies.” Yet another step in the cycle of neglect.
Zack, however, was lucky. He knew he could afford the treatment, so he went with the first option. He began treatment immediately, and got the first vaccination on the spot, without trekking back to Potosí and hunting the dog.
Neglected Tropical Diseases, and Neglected Infections of Poverty
Neglected Tropical Diseases weren’t always neglected. In the days of colonialism, there was a strong economic incentive for the richest nations of the world to develop effective treatments for tropical maladies. The economic and medical pressures of the colonial period also gave us the gin and tonic: soldiers of the British East India Company drank tonic with their gin, because the quinine in the tonic water prevented malaria.

British Library posed photograph of an Indian servant waiting on a European man, 1870s
When that era ended, neglect began. As the authors of a Doctors Without Borders paper wrote in 2002, “As Western interests drifted away from these regions, tropical diseases have become progressively neglected.” Other authors have cited post-colonial conflict in the latter half of the 20th Century as an additional reason for the halt of innovation. In any case, as the Doctors Without Borders wrote, “Despite an ever-increasing need for safe, effective, and affordable medicines for the treatment of these diseases, drug development has virtually stopped.”
As part of their analysis, they looked at all the new drugs that came out between 1975 and 1999. $307 million US were spent on non-infectious respiratory diseases, but only $3 million on tropical diseases. Of 1,393 new drugs brought to market in that time period, only 16 were for either tropical diseases — including malaria — or tuberculosis, and all were developed with public-sector support. “Not unexpectedly,” the authors wrote, “drug development outcomes closely follow the existence of viable markets.”
This lack of innovation has resulted in some serious shortcomings in medical technology. There’s still no vaccine for Dengue, nor treatment beyond palliative care. The current forms of treatment for African tryptanosomiasis, also known as sleeping sickness, are toxic, and resistant strains of the disease are gaining foothold. The recommended treatment for river blindness is a 10-15-year-long process, and can result in fatal complications in patients who also suffer from loa loa (which is common). Since there isn’t a better treatment, WHO’s recommends a protocol to manage these complications.
Rabies drugs are actually pretty good, relative to other Neglected Tropical Diseases — they’re relatively safe and they work, at least when properly administered. This is partly because it isn’t a strictly “tropical” disease. It can and has existed in more northern latitudes, and flourishes in the “tropics” mostly for economic reasons.
The problem with rabies treatments is that they are often prohibitively expensive, or poorly available where they are needed most. This is particularly problematic for such a time sensitive treatment, and such an underreported illness. (Poor diagnostics and slow, invisible illnesses are also pretty common among Neglected Tropical Diseases.)
Nonprofits are trying to pick up the slack in this market. Neglected Tropical Diseases are getting folded in to many HIV and malaria efforts and foundations. Efforts and investment are ramping up, and the pharmaceutical industry is chipping in by donating drugs and research. R&D is at about $500 million now, higher than it’s ever been, but still pretty tiny in an industry with an R&D expenditure of $130 billion.
The Bill and Melinda Gates Foundation bankrolled a $10 million dollar rabies research project from 2008-2013. There’s a lot of room for innovation in rabies — like in reducing the cost of treatment, or making preventative vaccination more widespread for humans in high-risk regions, or developing a diagnostic. But the chief focus of these research programs is canine vaccination, testing the feasibility of near-elimination through canine rabies control. While it’s suspected that this is the shortest and most cost-effective strategy to avoid future human death and suffering from rabies, there’s still a long way to go.
***

Zack, left, in Uspallata, Argentina wearing The Shirt
As Zack learned the hard way, rabies treatment can cause its own amount of suffering. Following his first injection, Zack’s body went to work fighting off the vaccine, and possibly small amount of the live virus, at the same time. He was headachey and nauseous, practically bedridden. For the next few weeks, instead of continuing on his travels he languished in La Paz, getting shots every five days.
Having researched online, he knew that rabies vaccines sometimes had these side effects. The Bolivian physician hadn’t given him the CDC-recommended shot of rabies antibodies before administering the vaccine, and Zack was worried that his immune system was collapsing. His physical strength gradually returned, but his spirit remained broken.
Crawling through a local market, between rabies shots, Zack found a t-shirt with a German shepherd on it. It looked like the dog that bit him. The shirt cost $1. He bought it, donned it, and over the period that followed, his strength returned. Armed with new health and new confidence, he left town, left Bolivia, and went on to have more — maybe somewhat questionable — adventures.
“I went to the Amazon even though I hadn’t been medicated against malaria,” Zack remembered, grinning. “My mom wanted to kill me.”
This post was written by Rosie Cima; you can follow her on Twitter here. To get occasional notifications when we write blog posts, please sign up for our email list